Inflammatory vs Mechanical Back Pain: Why the Difference Matters
Back pain is one of the most common reasons people see their GP — but not all back pain is the same. One of the most important distinctions we make in rheumatology is whether pain is mechanical or inflammatory. Identifying the correct type early can completely change the treatment plan, the long-term outlook, and how quickly patients feel better.
At my clinic, I regularly see patients who have lived with persistent back pain for months or years, often believing it is “just a strain,” “ageing,” or “a disc issue.” In many cases, their symptoms actually point towards an underlying inflammatory condition that needs a totally different approach.
This guide explains the key differences — and when to consider a rheumatology assessment.
What Is Mechanical Back Pain?
Mechanical back pain is the type most people are familiar with. It usually comes from the muscles, joints, ligaments, or discs in the spine.
Common causes
Muscle strain or spasm
Poor posture or prolonged sitting
Osteoarthritis (“wear and tear”)
Disc degeneration or bulging discs
Facet joint pain
Sciatica due to nerve compression
Typical features
Worse with activity, lifting, bending, or twisting
Better with rest
Pain may be sharp, localised, or radiate down the leg
Often triggered by a specific movement or injury
Morning stiffness is brief, usually minutes rather than hours
Treatment usually includes:
Physiotherapy
Exercise rehabilitation
Core strengthening
Posture changes
Pain relief when required
Mechanical pain is extremely common — and usually improves gradually with the right support.
What Is Inflammatory Back Pain?
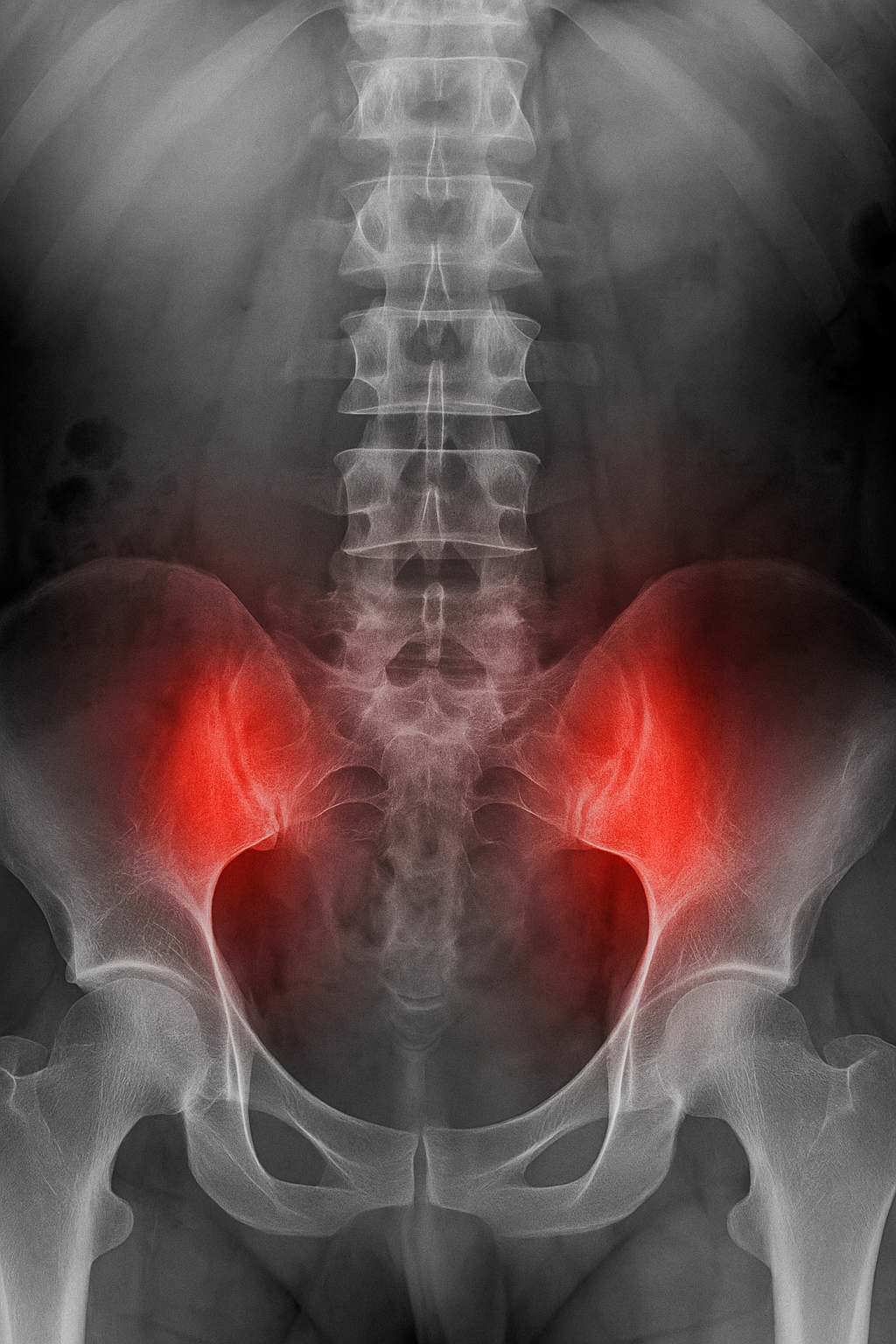
Inflammatory back pain comes from inflammation in the spine or sacroiliac joints (SI joints). This can be due to an underlying autoimmune condition, often in the spondyloarthritis (SpA) family.
The most important condition to identify early is:
Axial Spondyloarthritis (axSpA)
This includes the condition previously known as ankylosing spondylitis.
Inflammatory back pain often starts gradually, frequently in people under 45, and does not improve with rest.
Typical features
Patients often describe:
Pain and stiffness first thing in the morning, lasting >45 minutes
Improvement with movement and exercise, not rest
Night pain — waking in the second half of the night
Alternating buttock pain
Symptoms lasting more than 3 months
Onset typically under the age of 45
Other clues suggesting an inflammatory cause
A history of uveitis (eye inflammation)
Psoriasis
Crohn’s or ulcerative colitis
A family history of spondyloarthritis
Enthesitis (pain where tendons attach to bone, e.g. Achilles)
Good response to NSAIDs
Why early diagnosis matters
Left untreated, inflammation can cause:
Ongoing pain and stiffness
Loss of mobility
Structural changes to the spine
Fatigue and reduced quality of life
Modern treatments — including advanced biologic therapies — can transform symptoms and protect long-term spinal health.
How Inflammatory and Mechanical Back Pain Differ
Age of onset
Mechanical: Can occur at any age
Inflammatory: Often begins before age 45
Morning stiffness
Mechanical: Lasts only a few minutes
Inflammatory: Lasts more than 45 minutes
What improves symptoms
Mechanical: Rest usually helps
Inflammatory: Exercise and movement help
What worsens symptoms
Mechanical: Activity, bending or lifting
Inflammatory: Rest, inactivity or long periods sitting still
Night pain
Mechanical: Uncommon
Inflammatory: Common, especially in the second half of the night
Response to anti-inflammatory medication (NSAIDs)
Mechanical: May help slightly or not at all
Inflammatory: Often a dramatic improvement
Underlying cause
Mechanical: Muscles, joints, discs, posture or wear-and-tear
Inflammatory: Autoimmune inflammation of the spine or sacroiliac joints
How I Assess Back Pain in Clinic
During your consultation, I take a thorough history and examination, looking for subtle signs of inflammation that are easily missed. Depending on your symptoms, I may recommend:
MRI of the spine or sacroiliac joints (far more sensitive than X-ray)
Blood tests including inflammatory markers and HLA-B27
A tailored physiotherapy plan
Anti-inflammatory medications where appropriate
Early access to specialist biologic treatments if inflammation is confirmed
My approach is holistic: I look at your symptoms, lifestyle, sleep, mobility, and overall health — not just the spine in isolation.
When to See a Rheumatologist
You should consider a specialist review if you have:
Persistent back pain for >3 months
Morning stiffness lasting over 45 minutes
Pain that improves with exercise but returns at rest
Night pain that wakes you
Alternating buttock pain
A history of psoriasis, IBD, uveitis, or a family history of arthritis
Tried physiotherapy but symptoms remain unexplained
Early diagnosis can prevent years of discomfort and help you return to the activities you enjoy.
If This Sounds Like You, I Can Help
I offer rapid access appointments at the Physicians’ Clinic, the Devonshire Diagnostic Centre, and Chiswick Medical Centre for patients with back pain who want clarity and a personalised plan.
If you think your back pain may be inflammatory, early assessment can make a significant difference.
👉 Book an appointment
👉 Or contact my PA: DrSinghPA@ThePhysiciansClinic.co.uk / 0203 9855778
Please note, these posts are for general information only and do not constitute medical advice. Dr Singh would encourage you to speak to your healthcare professional to be assessed and managed for your specific symptoms.