What Is a DEXA Scan — and How Is It Used in Assessing Bone Health?
A DEXA scan is one of the most widely used investigations to assess bone strength and fracture risk. Many people are referred for a scan after a fracture, because of steroid use, early menopause, inflammatory or autoimmune disease, or as part of an osteoporosis assessment. Others receive results described as “borderline” or “worrying” without a clear explanation of what the numbers actually mean for them.
Understanding what a DEXA scan measures, how it is interpreted, and how it fits alongside clinical assessment, FRAX and other investigations is essential for making informed decisions about bone health.
What Does a DEXA Scan Measure?
DEXA stands for Dual-Energy X-ray Absorptiometry. The scan measures bone mineral density (BMD) — essentially how much mineral is packed into a specific area of bone.
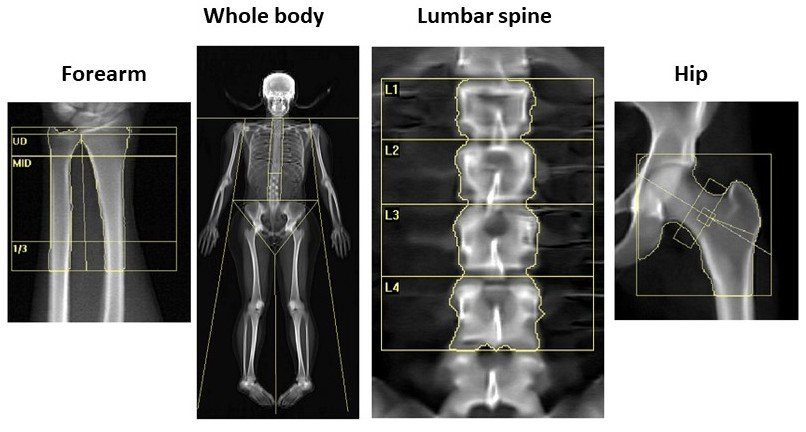
The scan most commonly assesses:
The lumbar spine
The hip
Occasionally the forearm
It uses a very low dose of X-rays and is quick, painless and non-invasive.
What Do the Results Mean?
DEXA results are reported as T-scores, which compare your bone density with that of a healthy young adult.
T-score ≥ –1.0
Bone density within the normal rangeT-score between –1.0 and –2.5
Osteopenia (mildly reduced bone density)T-score ≤ –2.5
Osteoporosis
While these thresholds are helpful, they are not the whole story. Two people with the same T-score may have very different fracture risks depending on age, fracture history, medications and other health factors.
What a DEXA Scan Can — and Cannot — Tell Us
What it does well
Quantifies bone density
Helps diagnose osteopenia or osteoporosis
Supports fracture risk assessment
Allows monitoring of bone density over time
What it does not show
Bone quality or micro-architecture
How quickly bone is being lost or gained
The cause of bone loss
Whether a fracture is imminent
For this reason, DEXA results should never be interpreted in isolation.
What Is FRAX and How Does It Fit In?
FRAX is a fracture risk assessment tool that estimates the 10-year probability of a major osteoporotic fracture (spine, hip, wrist or humerus) and of hip fracture specifically.
It incorporates clinical risk factors including:
Age and sex
Height and weight
Previous fractures
Parental history of hip fracture
Smoking
Steroid use
Rheumatoid arthritis
Alcohol intake
Secondary causes of osteoporosis
Hip bone density from DEXA can be added to FRAX, but it is not always required.
FRAX estimates risk; it does not make treatment decisions on its own. Clinical judgement remains essential.
Bone Turnover Markers: What Are They and When Are They Useful?
In some situations, blood tests known as bone turnover markers can provide additional information that a DEXA scan cannot.
Bone is a dynamic tissue, constantly being broken down and rebuilt. Bone turnover markers reflect the rate of bone resorption and formation, rather than bone density itself.
Commonly used markers include:
CTX (a marker of bone resorption)
P1NP (a marker of bone formation)
How Bone Turnover Markers Are Used
Bone turnover markers are not routinely required for everyone, but they can be helpful in selected situations, such as:
Assessing how active bone loss is
Supporting decisions in complex or borderline cases
Monitoring response to osteoporosis treatment
Checking adherence or biological response to therapy
Guiding sequencing of treatments, particularly in higher-risk patients
They provide dynamic information, whereas DEXA provides a static snapshot of bone density.
Importantly, bone turnover markers must be interpreted carefully, as levels can vary with time of day, recent fractures, kidney function and other factors.
Why Clinical Context Remains Central
Bone health is influenced by far more than a scan result. Important additional factors include:
Previous or recent fractures
Speed of bone loss
Age at menopause
Long-term steroid exposure
Inflammatory or autoimmune disease
Kidney and gastrointestinal health
Falls risk, muscle strength and balance
A specialist assessment brings these factors together, helping to avoid both over-treatment and under-treatment.
Patients are often reassured to learn that:
A “borderline” DEXA result does not automatically mean medication is required
A normal scan does not guarantee low fracture risk
Management decisions are individualised and evidence-based
How DEXA and Related Tests Guide Management
Taken together, DEXA, FRAX and — where appropriate — bone turnover markers help guide decisions around:
Lifestyle and exercise interventions
Calcium and vitamin D optimisation
Monitoring without immediate medication
Anti-resorptive therapies
Anabolic treatments in selected high-risk individuals
Long-term treatment sequencing
For patients at very high fracture risk, these tools help inform a structured and forward-looking management plan.
Why Consultant Rheumatologist Assessment Can Be Helpful
Interpreting bone density results, fracture risk and additional investigations requires experience, particularly when findings do not fit neatly into guidelines or when decisions about advanced therapies are being considered.
A specialist assessment allows time to:
Explain results clearly and in context
Integrate scans, blood tests and clinical history
Clarify true fracture risk
Develop a personalised, guideline-based plan including accessing specialist medication
Provide continuity and follow-up over time
Many patients value having a clear explanation of why a particular approach is recommended and what the longer-term plan looks like.
Trusted Patient Information Resources
For further reliable, patient-friendly information:
Royal Osteoporosis Society (UK)
https://theros.org.ukNHS – Osteoporosis
https://www.nhs.uk/conditions/osteoporosisFRAX® fracture risk assessment tool
https://www.sheffield.ac.uk/FRAXNational Osteoporosis Guideline Group (NOGG)
https://www.nogg.org.uk
In Summary
A DEXA scan measures bone mineral density
Results are reported as T-scores
FRAX estimates fracture risk using clinical factors, with or without DEXA
Bone turnover markers can provide additional, dynamic information in selected cases
None of these tools should be used in isolation
Specialist interpretation helps ensure appropriate and personalised care
Used together and interpreted carefully, these assessments support informed, evidence-based decisions about bone health and fracture prevention.
Related Reading
Understanding bone density is only one part of assessing fracture risk. Many patients find it helpful to explore how DEXA results fit into broader osteoporosis care and treatment decisions:
Osteoporosis: Understanding Bone Strength, Fracture Risk and Treatment Options
Explains how osteoporosis is diagnosed, why fractures occur, and how treatment decisions are made beyond bone density alone.Romosozumab (Evenity®) in Osteoporosis: When and Why It Is Used
Outlines when bone-building treatments may be considered for people at very high fracture risk, in line with NICE, NOGG and Royal Osteoporosis Society guidance.
These articles expand on how scan results, fracture history and clinical assessment come together to guide personalised osteoporosis management.
Please note, these posts are for general information only and do not constitute medical advice. Dr Singh would encourage you to speak to your healthcare professional to be assessed and managed for your specific symptoms.